Colorectal Cancer Prevention
You can seriously diminish the chances of getting colorectal cancer by taking some precautions.
-
Identifying Risk Factors
Screening
Treatment
Identifying Risk Factors
Preventing cancer from occurring in the first-place-primary prevention is the most definitive way to lessen the burden of cancer. Developing primary prevention strategies requires knowing something about the causes or risk factors associated with the cancer. If the cause or risk factor can be eliminated or reduced, prevention is possible.
While the exact cause of each individual’s colorectal cancer is indeed difficult to determine, there are certain know factors that can put people at risk.
Anything that increases your chance of developing colorectal cancer is called a risk factor; anything that decreases your chance of developing cancer is called a cancer protective factor.
So, we may lower our risk by avoiding risk factors and by increasing protective factors.
You are more at risk of getting cancer if you have one or more risk factors. This doesn’t mean that you will definitely get colorectal cancer. Equally, if you don’t have any risk factors, it doesn’t mean you can’t get cancer.
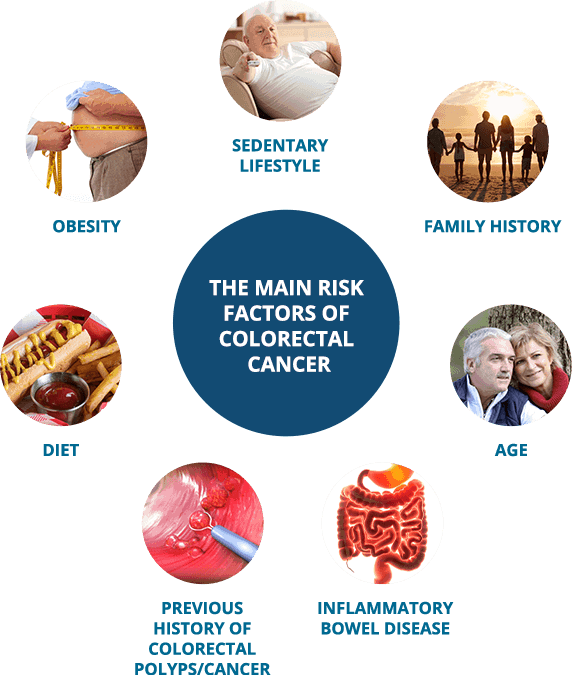
The Following Risk Factors Increase the Risk of Colorectal Cancer:
- Ageing: the risk of colorectal cancer increases as a person gets older; Most cases occur in the 60s and 70s, however whilst only 2.5% of cases of colorectal cancer occur in the under 50’s it is on the increase. A significant proportion of young people who are diagnosed with colorectal cancer have no hereditary risk or family history of the disease.
- Lifestyle-related risk factors:
- Diet:
- A low-fiber, low in fruit and vegetables and high-fat diet
- High consumption of alcohol
- Obesity (overweight)
- Sedentary lifestyle
- Smoking
- Diet:
- Previous history of colorectal polyps: Individuals who have previously been diagnosed and treated for colorectal polyps are at increased risk for developing colorectal cancer in the future. Women who have had cancer of the ovary, uterus or breast have a higher than average risk of developing colorectal cancer.
- Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis
- Family history
- Certain hereditary syndromes
Are You at a Higher Risk of Developing CRC?
People who have certain genetic colorectal cancer syndromes and those who have inflammatory bowel disease (IBD) are considered to be at higher risk for colorectal cancer. Also, if you have a history of previous CRC you are at higher risk.
Your physician can guide you and your family members through a risk assessment, screening and monitoring to reduce colorectal cancer risk.
Familial Risks

A small percent of individuals (approximately 20 %) with colorectal cancer have a hereditary form inherited from one of their parents. In those families the chance of developing colorectal cancer is significantly higher than in the average person. These hereditary cancers typically occur at an earlier age than sporadic (non-inherited) cases of colorectal cancer.
Hereditary cancer is caused by some DNA mutations (changes) that can be passed on in families and are found in all of a person’s cells.
Many of these DNA changes and their effects on the growth of cells are now known.
Familial Adenomatous Polyposis (FAP)
Individuals with this condition have a mutation or a loss of the FAP gene, which causes hundreds or thousands of polyps to grow in the large intestine at a young age. Cancer may develop in one or more of these polyps before the age of 40 and sometimes as early as age 20.
Lynch syndrome, also called Hereditary Non-polyposis Colorectal Cancer (HNPCC)
Individuals with this condition have certain gene mutations (changes) that cause failure of the DNA repair mechanisms, like MLH1, MSH2, MLH3, MSH6, PMS1, and PMS2. These changes can allow DNA errors to go unfixed and cause colorectal cancer.
If you have an inherited syndrome you may be referred to a genetic counsellor. A genetic counsellor can talk with you about the possibilities that your children/siblings/parents have the same gene abnormalities and may recommend that they are screened.
Obesity
Overweight and obesity are defined, by the World Health Organization, as abnormal or excessive fat accumulation that presents a risk to health. (www.who.int)
Obesity can be measured, in a crude way, by calculating the body mass index (BMI):
Body mass index (BMI) applies to both adult men and women and is the calculation of body weight in relation to the height.
You can calculate your bodyweight with the following formula:
Metric BMI Formula: BMI = weight (kg) / [height (m)]2
A person with a BMI of 30 or more is generally considered obese. A person with a BMI equal to or more than 25 is considered overweight. Persons with a BMI equal or less than 25 are having a normal weight.
The result is only an estimate and it doesn’t take into account age, ethnicity, gender and body composition. We recommend you also to check your waist measurement and other risk factors.

Please confirm if you accept our tracking cookies. When declining the cookies, you can continue visiting the website without sending data to third party services. Read our complete cookie statement here.
